Endocrine glands and organs play a vital role in human health by producing compounds that regulate the functioning of various organs and tissues at the cellular level. Best known examples of this include insulin, which helps sugar to penetrate cells, thyroid hormones that stimulate metabolism, and several hormones produced by the adrenal glands responsible for regulating fat metabolism, stress and overall hydration to name a few. By far the most common endocrine dysfunction, affecting an estimated 425 million individuals worldwide, is diabetes.
What is diabetes?
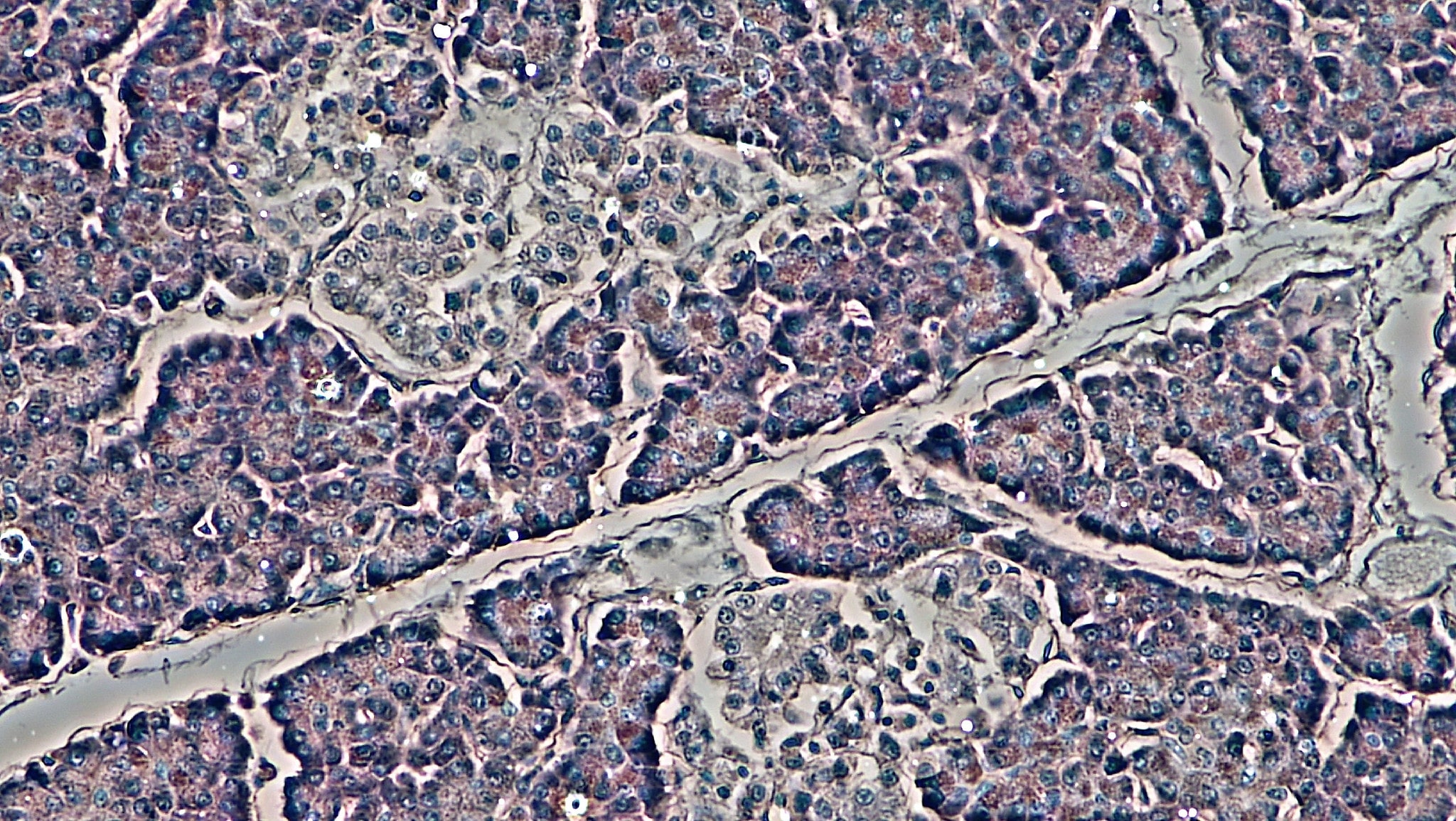
Diabetes is a metabolic syndrome caused by a deficiency in insulin, a pancreatic hormone that plays a crucial role in the uptake of glucose by every cell of the body. Diabetes is therefore characterized by abnormally high glucose levels in the blood. The two common forms of diabetes are caused by either a decline in the actual production of insulin (Type 1) or a diminished response by the cells to insulin (Type 2).
Elevation in blood glucose levels leads to the glycation of various blood proteins, which in turn leads to the formation of compounds called “Advanced Glycation End products” (AGEs). AGEs are responsible for most of the problems associated with diabetes.[1]
There is no solution
Although diabetes has been relatively well-controlled since insulin became medically available in 1921, there is still no cure for the disease. Diabetes and its complications altogether constitute the number 1 cause of morbidity worldwide, including retinopathy (degeneration of the retina), kidney failure, heart disease, neuropathy (loss of sensation), vascular degeneration (poor circulation), diabetic wounds and ultimately amputation. While controlled, it remains a huge problem.
The Stem Cell Promise
As soon as it was discovered that stem cells can transform into cells of various tissues, scientists began to look at the potential application of stem cells to diabetes. Rapidly, bone marrow stem cells were shown to have the ability to transform into insulin-producing cells.[2] But more importantly, in a landmark study, scientists demonstrated that this phenomenon takes place naturally in the pancreas, in a living organism. Stem cells have the ability of naturally leaving the bone marrow, migrating into the pancreas and transforming into normal insulin-producing pancreatic cells.[3] Stem cells were also documented to form new blood vessels in the pancreas and to improve pancreatic function.[4]
Using Stem Cells to Improve Blood Glucose
As the concept of Endogenous Stem Cell Mobilization (ESCM) evolved and gained interest, many scientific groups investigated whether stimulating the release of one’s own stem cells could improve pancreatic function. Using various protocols, ESCM was documented to harbor great potential in improving pancreatic function and helping to normalize blood glucose levels.[5][6][7] ESCM was also documented to have beneficial effects on problems associated with diabetes.[8][9][10]
Check more Organ Systems in our interactive tool
Stem Cell Number and Pancreatic Function
As stem cells were being investigated to help improve pancreatic function, it was discovered that as people advance through the various phases of the development of diabetes, they have fewer and fewer circulating stem cells.[11] The same observation was made with diabetic complications linked to vascular health and kidney function.[12][13] In other words, people developing diabetes and its complications have, on average, fewer stem cells than healthy individuals.
But this problem was in fact dual, meaning that while pancreatic function was declining because of a decline in the number of circulating stem cells, the consequent increase in blood glucose was creating AGEs, which in turn reduced the ability of the bone marrow to release stem cells.[14][15] In other words, once diabetes starts to develop, it is the whole body that experiences a reduced ability to release stem cells and therefore to repair the very condition causing diabetes and to stay healthy. So, increasing the number of circulating stem cells becomes even more important as a general health strategy for diabetics.
Thyroid and Adrenal Functions
Likewise, although more research needs to be done in this area, many studies have documented the ability of bone marrow stem cells to transform into functional cells of both the thyroid and adrenal glands, and to improve functions of these tissues.[16][17][18][19]
Conclusion
Whether it improves the actual function of the pancreas or simply helps the whole body renew and maintain optimal health, supporting the natural release of one’s own stem cells using a natural stem cell enhancer can bring significant benefits to individuals challenged with problems of the endocrine system.
Sources
[1] Advanced glycation end products and diabetic complications.
Singh VP, Bali A, Singh N, Jaggi AS. Korean J Physiol Pharmacol. 2014 Feb;18(1):1-14.
[2] Differentiation of rat marrow mesenchymal stem cells into pancreatic islet beta-cells.
Chen LB, Jiang XB, Yang L. World J Gastroenterol. 2004 Oct 15;10(20):3016-20.
Ianus A, Holz GG, Theise ND, Hussain MA. J Clin Invest. 2003 Mar;111(6):843-50.
[4] Recruitment of bone marrow-derived endothelial cells to sites of pancreatic beta-cell injury.
Mathews V, Hanson PT, Ford E, Fujita J, Polonsky KS, Graubert TA. Diabetes. 2004 Jan;53(1):91-8.
Gol’dberg ED, Dygai AM, Zhdanov VV, Zyuz’kov GN, Ermakova NN, Vetoshkina TV, Fomina TI, Ermolaeva LA, Dubskaya TY. Bull Exp Biol Med. 2008 Oct;146(4):543-6.
Hasegawa Y, Ogihara T, Yamada T, Ishigaki Y, Imai J, Uno K, Gao J, Kaneko K, Ishihara H, Sasano H, Nakauchi H, Oka Y, Katagiri H. Endocrinology. 2007 May;148(5):2006-15.
Voltarelli JC, Couri CE, Stracieri AB, Oliveira MC, Moraes DA, Pieroni F, Coutinho M, Malmegrim KC, Foss-Freitas MC, Simões BP, Foss MC, Squiers E, Burt RK. JAMA. 2007 Apr 11;297(14):1568-76.
Tian B, Li XX, Shen L, Zhao M, Yu WZ. Chin Med J (Engl). 2010 Aug;123(16):2265-8.
Cruciani M, Lipsky BA, Mengoli C, de Lalla F. Diabetes Care. 2005 Feb;28(2):454-60.
Iwamoto S, Lin X, Ramirez R, Carson P, Fiore D, Goodrich J, Yufit T, Falanga V.
Int J Low Extrem Wounds. 2013 Dec;12(4):256-64.
Fadini GP, Boscaro E, de Kreutzenberg S, Agostini C, Seeger F, Dimmeler S, Zeiher A, Tiengo A, Avogaro A. Diabetes Care. 2010 May;33(5):1097-102.
Fadini GP, Sartore S, Albiero M, Baesso I, Murphy E, Menegolo M, Grego F, Vigili de Kreutzenberg S, Tiengo A, Agostini C, Avogaro A. Arterioscler Thromb Vasc Biol. 2006 Sep;26(9):2140-6.
[13] Decreased circulating CD34+ cells are associated with progression of diabetic nephropathy.
Makino H, Okada S, Nagumo A, Sugisawa T, Miyamoto Y, Kishimoto I, Kikuchi-Taura A, Soma T, Taguchi A, Yoshimasa Y. Diabet Med. 2009 Feb;26(2):171-3.
[14] Diabetes impairs hematopoietic stem cell mobilization by altering niche function.
Ferraro F, Lymperi S, Méndez-Ferrer S, Saez B, Spencer JA, Yeap BY, Masselli E, Graiani G, Prezioso L, Rizzini EL, Mangoni M, Rizzoli V, Sykes SM, Lin CP, Frenette PS, Quaini F, Scadden DT.
Sci Transl Med. 2011 Oct 12;3(104):104ra101.
[15] Diabetes impairs stem cell and proangiogenic cell mobilization in humans.
Fadini GP, Albiero M, Vigili de Kreutzenberg S, Boscaro E, Cappellari R, Marescotti M, Poncina N, Agostini C, Avogaro A. Diabetes Care. 2013 Apr;36(4):943-9.
[16] Thyroid regeneration: how stem cells play a role?
Kimura S. Front Endocrinol (Lausanne). 2014 Apr 14;5:55.
[17] Bone marrow stem cells repopulate thyroid in X-ray regeneration in mice.
Mikhailov VM, Sokolova AV, Serikov VB, Kaminskaya EM, Churilov LP, Trunin EM, Sizova EN, Kayukov AV, Bud’ko MB, Zaichik ASh. Pathophysiology. 2012 Feb;19(1):5-11.
[18] Differentiation of mesenchymal stem cells into gonad and adrenal steroidogenic cells.
Yazawa T, Imamichi Y, Miyamoto K, Umezawa A, Taniguchi T. World J Stem Cells. 2014 Apr 26;6(2):203-12.
[19] New directions for the treatment of adrenal insufficiency.
Ruiz-Babot G, Hadjidemetriou I, King PJ, Guasti L. Front Endocrinol (Lausanne). 2015 May 6;6:70.